Physiotherapy for Hip Pain: What You Need to Know
Restore Mobility, Relieve Pain, and Reclaim Your Active Life
Hip pain can be frustrating and limiting. Whether you’re an athlete, a working professional, or a senior citizen, it can affect your ability to move freely, exercise, or even carry out daily tasks. Fortunately, physiotherapy for hip pain offers a non-invasive, effective way to manage the discomfort and restore function.
In this blog, we’ll break down:
- The common causes of hip pain
- How physiotherapy helps
- Key treatment techniques
- FAQs and expert tips to get you started on the road to recovery

Understanding Hip Pain
Your hip joint plays a vital role in keeping you upright, mobile, and active. It’s one of the strongest joints in the body but also one of the most prone to wear and tear, especially due to age, injuries, or repetitive stress.
Common Causes of Hip Pain:
- Osteoarthritis – Degeneration of cartilage, causing stiffness and swelling
- Tendinitis – Inflammation of tendons due to overuse
- Bursitis – Inflamed fluid sacs causing sharp, stabbing pain
- Hip Fractures – Common in older adults due to falls
- Labral Tears – Cartilage damage inside the hip joint
- Muscle Strains – Pulled or overstretched muscles around the hip
Each of these conditions can lead to decreased mobility and ongoing discomfort. That’s where physiotherapy steps in.

Why Physiotherapy is Key to Hip Pain Relief
Physiotherapy doesn’t just treat symptoms, it treats the root cause of your hip pain. It’s a personalized, movement-based therapy that restores mobility, improves strength, and enhances your overall quality of life.
How Physiotherapy Helps:
- Pain Relief – Through modalities like heat, cold packs, ultrasound, and TENS
- Strength Training – Builds support in muscles around the hip
- Flexibility & ROM Exercises – Improves joint function and daily movements
- Posture & Gait Correction – Reduces strain caused by incorrect body mechanics
- Education & Lifestyle Tips – Learn habits and movements that protect your hips

Top Physiotherapy Techniques for Hip Pain
Here are some techniques used by physiotherapists at FitoFine and other reputed clinics:
1. Strengthening Exercises
- Clamshells – Activate glutes and stabilize hips
- Bridges – Strengthen lower back and hamstrings
- Step-Ups & Squats – Build lower body strength
2. Stretching & Flexibility
- Hip Flexor Stretch – Reduces tightness in the front hip
- IT Band Stretch – Releases tension on the side of the leg
- Hamstring Stretch – Improves flexibility behind the thigh
3. Manual Therapy
- Hands-on mobilization of joints and muscles to reduce stiffness
- Helps improve blood flow and release muscle knots
4. Electrotherapy
- TENS or ultrasound therapy to manage chronic pain
- Reduces inflammation and accelerates healing
Additional Benefits of Physiotherapy
- Better Mobility – Get back to walking, climbing stairs, or exercising without pain
- Avoid Surgery – Many patients delay or avoid surgery with consistent therapy
- Injury Prevention – Strengthening and correcting movement patterns to protect your joints
- Improved Confidence – Move freely, without the fear of pain or injury

Prevalence
- Highly variable due to differences in definitions (radiographic, symptomatic, self-reported).
- 2011 meta-analysis (Pereira et al):
- Prevalence ranged 0.9%–45%.
- Similar prevalence in men (11.5%) and women (11.6%) (unlike knee OA which is more common in women).
- Incidence data limited: 3.8% over 10 years – 33% over 8 years.
- Public health problem expected to increase with ageing populations.
Burden
- Leading cause of musculoskeletal pain and disability (Vos et al, 2012).
- Symptoms: persistent pain, mobility issues, difficulty with daily tasks, anxiety, depression, fatigue, and poor sleep.
- Major economic burden: conservative & surgical treatment costs, productivity loss, rising hip replacement surgeries (even in younger patients).
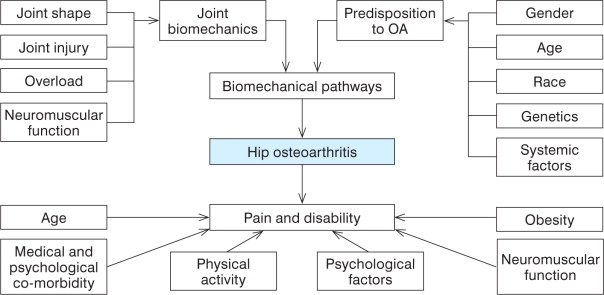
Risk Factors & Natural History
- Joint-specific risks: developmental hip disorders (dysplasia, Perthes, SCFE), femoroacetabular impingement.
- Systemic risks: age, obesity, occupational heavy lifting, high-impact sports, leg length discrepancy, ethnicity (higher in Caucasians).
- Progression:
- Radiographic worsening is common but variable.
- Predictors: age, baseline hip pain, radiographic features (Wright et al, 2009).
- Pain & function may remain stable for ≤3 years but decline with longer follow-up.
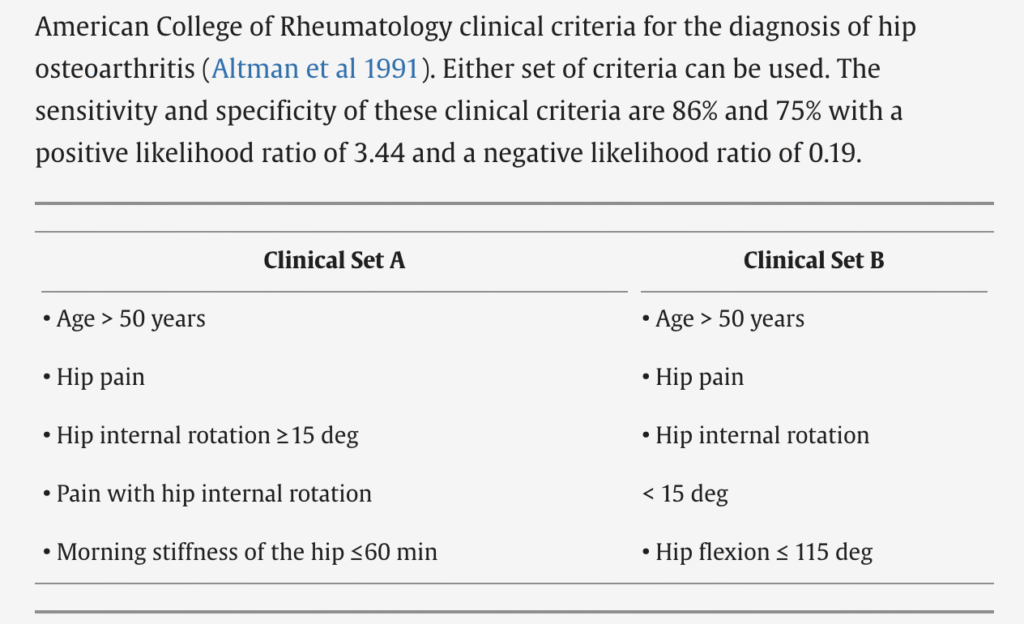
Diagnosis
- Usually based on history & clinical exam (avoid unnecessary X-rays).
- ACR Criteria (Altman et al, 1991):
- Clinical Set A: Age >50, hip pain, internal rotation ≥15°, pain with IR, morning stiffness ≤60 min.
- Clinical Set B: Age >50, hip pain, IR <15°, hip flexion ≤115°.
- Imaging:
- X-ray → moderate/severe disease (joint space narrowing, osteophytes, sclerosis).
- MRI → early cartilage/bone changes.
Assessment
- Subjective: pain, stiffness after rest, psychosocial impact.
- Objective: ↓ range of motion, hip/thigh muscle weakness (esp. abductors, quadriceps), altered gait, balance deficits.
- Validated outcome tools: WOMAC, Harris Hip Score, Lower Extremity Functional Scale, 30s Chair Stand, 40m Walk Test, Stair Climb Test.
Principles of Management
- Guidelines recommend:
- Conservative first: education + exercise (core treatments).
- Weight loss (if overweight).
- Multimodal, patient-centred, shared decision-making.
- Drugs and surgery: small/modest benefits, higher risks.
Physiotherapy & Non-drug Interventions
Education & Self-Management
- Key for self-care & lifestyle modification.
- Topics: OA knowledge, active lifestyle, weight management, joint protection, coping strategies, stress management.
- Effectiveness: modest (small benefits for pain/anxiety, mixed for function).
Exercise Therapy
- Integral regardless of age, severity, or comorbidities.
- Types studied: strengthening, ROM, balance, Tai Chi, aquatic exercise.
- Evidence:
- Effects on pain = small.
- Effects on function = small to moderate (greater than for pain).
- Aquatic exercise recommended as alternative.
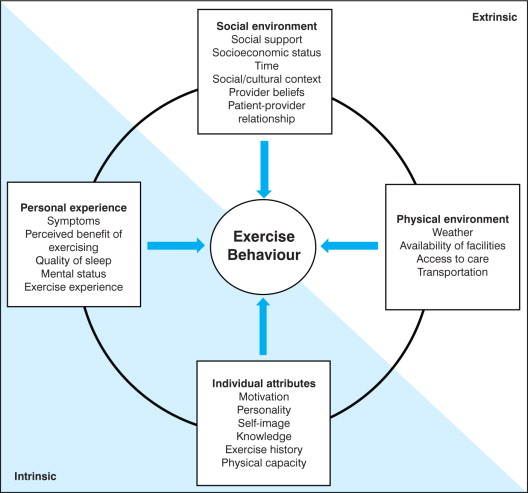
- Long-term adherence is essential but often poor.
Behavioural Graded Activity
- Focuses on reinforcing healthy behaviors & physical activity.
- Evidence:
- Improves activity levels & exercise adherence.
- May delay hip replacement surgery.
- Cost comparable to usual exercise therapy.
Research Gaps
- Lack of large, hip-specific RCTs.
- Most evidence extrapolated from knee OA studies.
- Need for:
- Tailored exercise interventions for hip OA.
- Studies on long-term adherence & functional outcomes.
- Exploration of psychosocial and neuromuscular factors.
Key Takeaway:
Hip OA is a growing global problem with significant personal and economic burden. Current best practice = education + exercise + weight management, but benefits are modest and evidence is limited compared to knee OA. More targeted research is urgently needed.
How Long Will Physiotherapy Take?
Recovery time varies, but most patients:
- Notice improvements within 2–3 weeks
- Achieve major relief by 4–6 weeks
- Require long-term sessions only for chronic or severe conditions
Your physiotherapist will track your progress and adjust the treatment accordingly.

FAQs About Physiotherapy for Hip Pain
Q1: Can physiotherapy cure arthritis?
Not a cure, but it can significantly reduce pain and stiffness, improve joint function, and delay the need for surgery.
Q2: How often should I visit the physiotherapist?
Usually 2-3 sessions per week at the beginning. As you progress, this may be reduced to once a week or bi-weekly.
Q3: Is physiotherapy painful?
Some exercises may cause mild discomfort, but a good therapist adjusts the plan to your tolerance.
Q4: Can I exercise with hip pain?
Yes, but choose low-impact activities like swimming or cycling. Avoid anything that causes sharp pain.
Q5: What if physiotherapy doesn’t work?
If your condition doesn’t improve, your therapist may suggest advanced treatments or refer you for a surgical consult as a last resort.
Start Your Journey to Pain-Free Hips with FitoFine
At FitoFine Physiotherapy Clinic, we specialize in treating hip pain with customized, research-backed therapies. Our expert team is committed to helping you return to a life full of movement, pain-free and strong.
Clinic Details:
Hours: Mon–Sat: 5:00 PM – 10:00 PM | Sunday: Closed
Email: fitofine.in@gmail.com
Website: www.fitofine.com
Phone/WhatsApp: +91 6295115701
FitoFine: Helping You Live a Life with Less Pain and More Movement.



